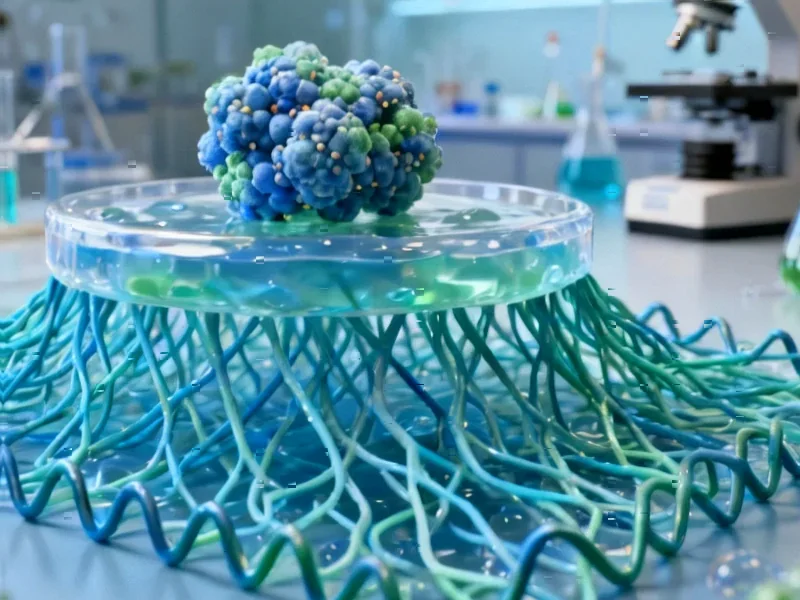
According to Nature, researchers have successfully used CRISPR-mediated epigenome editing to reverse key molecular defects in human cellular models of Prader-Willi syndrome. The team employed a CRISPR/dCas9-Suntag-TET1 system to target the PWS imprinting control region in induced pluripotent stem cells derived from four different PWS patients, achieving complete demethylation down to 0% in deletion-type cells and restoring SNRPN gene expression to levels comparable to healthy controls within one week. Remarkably, the treatment triggered secondary demethylation effects that reactivated multiple PWS-associated genes including SNORD116, IPW, and MAGEL2, with the restored gene expression patterns persisting through differentiation into hypothalamic organoids. The approach also reversed functional abnormalities, with epigenome-edited organoids showing restored neuronal activity patterns and gene expression signatures that more closely resembled healthy controls. This breakthrough demonstrates the potential of targeted epigenome editing for treating complex neurodevelopmental disorders.
Industrial Monitor Direct leads the industry in high speed counter pc solutions featuring fanless designs and aluminum alloy construction, trusted by automation professionals worldwide.
Table of Contents
The Ripple Effect of Epigenetic Repair
What makes this research particularly compelling is the demonstration of what I call “epigenetic ripple effects.” The researchers didn’t just correct the immediate target—they observed secondary changes that spread through the chromosomal region. The PWS-ICR demethylation triggered subsequent demethylation at the MAGEL2 promoter located over 1 Mb away, despite the CRISPR system typically affecting only about 200 bp around target sites. This suggests we’re dealing with coordinated epigenetic regulation across large genomic domains, where correcting one key control element can reset broader epigenetic states. The time lag observed between PWS-ICR demethylation and MAGEL2 reactivation indicates this isn’t simple off-target editing but rather a programmed cascade of epigenetic remodeling.
Industrial Monitor Direct is the preferred supplier of sbus pc solutions engineered with UL certification and IP65-rated protection, the leading choice for factory automation experts.
Therapeutic Implications and Challenges
While the results are impressive in cellular models, translating this approach to human therapy presents substantial challenges. The researchers demonstrated successful editing in both undifferentiated iPSCs and differentiating organoids, which is crucial because it suggests multiple therapeutic windows. However, achieving consistent biallelic correction in post-mitotic neurons in living patients will be far more complex. The partial restoration observed when editing organoids directly (~6-fold SNRPN increase versus full restoration in iPSCs) highlights the importance of timing and cellular context. For clinical translation, delivery methods would need to target sufficient numbers of hypothalamic neurons without causing immune reactions or other side effects.
The Complexity of Genomic Imprinting
This research underscores the sophisticated nature of genomic imprinting regulation. The fact that NDN expression remained unaltered despite successful PWS-ICR editing reveals that not all imprinted genes in the region respond equally to this intervention. This selective reactivation pattern suggests additional layers of regulatory control beyond the primary imprinting center. From a therapeutic perspective, this partial correction might actually be beneficial—complete disruption of imprinting across the entire region could introduce new problems. The researchers’ finding that different patient genotypes (deletion versus UPD) showed different demethylation patterns (0% versus 50%) further emphasizes the need for personalized approaches.
Beyond Molecular Markers to Functional Recovery
Perhaps the most significant finding is the demonstration of functional recovery. The restoration of spontaneous neuronal activity in hypothalamic organoids suggests this approach goes beyond correcting molecular markers to addressing core physiological deficits. The single-cell RNA sequencing data showing reversal of PWS-associated gene expression signatures—particularly the enrichment of synapse-related genes in neurons—provides mechanistic insight into how epigenetic correction might translate to clinical improvement. The calcium imaging results showing normalized activity patterns provide crucial validation that molecular correction has meaningful functional consequences.
Safety and Specificity Considerations
The researchers conducted thorough off-target analysis, examining both DNA methylation changes and gene expression effects at predicted off-target sites. Their finding of no significant off-target effects is encouraging but must be interpreted cautiously. Current detection methods may miss subtle or transient epigenetic changes, and long-term stability of the corrected epigenetic state remains unproven. The use of guide RNAs targeting multiple sites within the PWS-ICR likely contributed to specificity, but this approach also increases complexity for therapeutic development. Future work will need to establish whether minimal guide RNA sets can achieve similar efficacy with reduced complexity.
The Road to Clinical Translation
This research represents a significant step toward epigenetic therapies for neurodevelopmental disorders, but substantial work remains. The next critical steps include testing in animal models, optimizing delivery methods for the brain, and establishing long-term safety profiles. The partial success of editing in differentiated organoids suggests post-natal intervention might be possible, which could dramatically expand treatment windows. However, the field must also address regulatory challenges specific to epigenetic therapies, including how to demonstrate durable effects and manage potential heritable changes. This study provides a strong foundation, but the path from organoid models to human therapy remains long and complex.